“I have never dealt with an easier transcription service. Rapid turnaround time for dictations and an easy to contact customer service.”
Powered by AI. Perfected by Experts.
Dictate. Let ZyDoc do the rest.
ZyDoc enables physicians to effortlessly populate the appropriate sections of their EHR with flawless clinical notes using a dictation-based, mobile-friendly system of medical documentation.

than typing & clicking
for STAT dictation jobs
versus speech recognition
AI alone isn’t enough.



Auto-populate your EHR instantly with expert-corrected clinical notes. No workflow changes.

Supporting all major platforms
including Athena Health, AdvancedMD, DRChrono, ECW, & more.





One platform. Your workflow.
Materially lower than common seat prices for DAX (~$600+), Suki (~$299–$399), DeepScribe (~$500–$750), etc.
Guaranteed ≧ 99.6% accuracy.
Create a Granular quality dial: add human QA at a rate of $0.10/line; perfect for high-risk or specialty notes.
Turn on the $75/mo EHR add-on where needed; no more copy/paste into your EHR.
- Direct EHR Insertion, NO COPY & PASTE
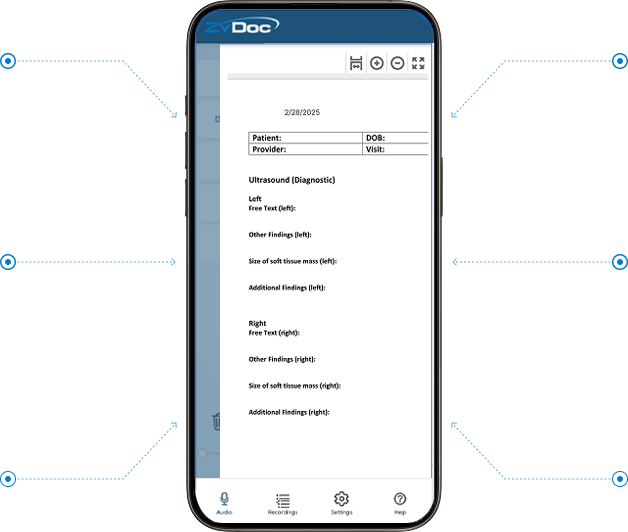
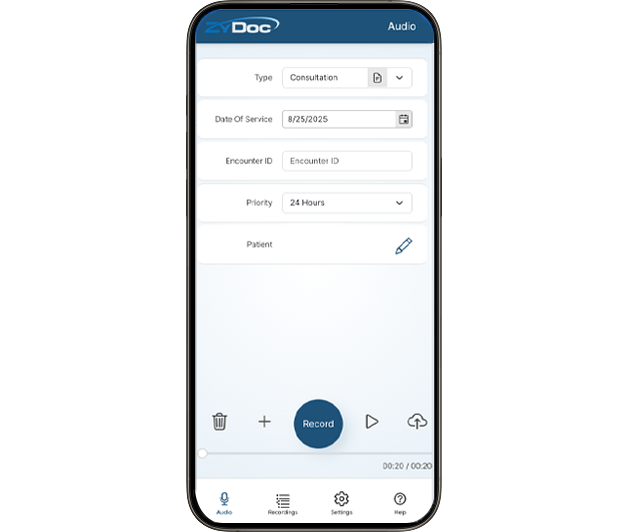
- ZyDoc smartphone recording app
- U.S. based, HIPAA compliant and background checked medical language specialist editors
- Guaranteed accuracy - No other company can guarantee 99.6+% accuracy
- Proprietary, specialty specific language models
- <1 hour max. turnaround time for dictations that are <15 minutes
- 1-800 phone hospital/ASC dictation recording
- Audit trail
- Letterheads
- Job-type templates
- Faxing
- Default normals and frequently-used phrase insertions
- Handheld digital recorder submission Software
- Telephone or email support 24/7/365
- HIPAA security w/ geolocation audit log
- Closed-loop feedback and quality assurance process
- Hallucinations, omissions and error correction
- Simplified patient summary
- Translation of simplified patient summary

* $0.10 per line ≈ ~$1.00 per minute of dictation (assuming the industry-standard 65-character line and typical physician speech rate). A ~2-minute clinic note is about $2, a 3-minute note $3, and a 5-minute note $5.
Quick spend snapshots (rule-of-thumb):
- Average clinic (20 notes/day × ~2 min): ~$40/day → ~$800/month (20 clinic days)
- Light day (12 notes × ~1.5 min): ~$18/day → ~$360/month
Busy day (30 notes × ~2.5 min): ~$75/day → ~$1,500/month
** 1x Data charges vary pending your preferred EHR. ZyDoc credits all integration fees at-cost directly to your client account as an incentive to integrate for direct insertion-level features. This means there’s no integration fees for ZyDoc after only a few months of service.
Let ZyDoc do the rest.
Say it once. Get it done.
Smarter Documentation for Every Care Setting
ZyDoc isn’t just transcription — it’s an end-to-end documentation solution tailored to the unique needs of physicians, hospitals, and surgery centers. Our blend of AI + expert human review ensures accuracy, speed, and seamless EHR integration, so you can focus on what matters most: patient care.
Physicians & Specialty Practices
Spend more time with patients, not paperwork. ZyDoc helps streamline:
- Follow-up visits – speed up repetitive documentation while maintaining accuracy.
- Initial consultations – capture complete histories without typing.
- Annual physicals – ensure thorough, accurate documentation every time.
- Clinic & chart notes – reduce errors and improve continuity of care.

Hospitals
Handle complex workflows with confidence. ZyDoc supports:
- Follow-up notes & discharge summaries – streamline transitions of care and improve patient safety.
- Consultations & clinic notes/reports – get consistent, error-free records across departments.
- Chart notes – ensure compliance and reduce physician workload.
- Operation notes & reports – capture critical details with precision.

Ambulatory Surgery Centers (ASCs)
Simplify high-volume surgical documentation. ZyDoc delivers:
- Discharge summaries – reduce delays and enhance care coordination.
- Operation notes & reports – complete and accurate, ready for billing.
- Follow-up appointment notes – faster documentation for post-op care.
Trusted and Tested
Why Doctors Choose ZyDoc Medical Transcription.
“It has been really easy to get ZyDoc up and running at our new multi-specialty center. The team at Zydoc has been top quality and easy to work with and the physicians are finding the service very easy to use.
"Professional service, fast turnaround, very efficient and excellent value for money!"
Support for every practice
ZyDoc supports physicians in the following disciplines through all major procedures and speciality practice settings:
local anesthesia, regional anesthesia, general anesthesia, spinal anesthesia, epidural anesthesia.
diagnosis, risk assessment, preventative appointments, invasive procedures, heart failure management, interventional cardiology, cardiac rehabilitation, cardiac screenings.
realignment, spinal mobilization, myofascial release, cervical spine manipulation, therapeutic exercise and stretches, soft tissue manual therapy, physical therapy.
consultations, skin grafts, laser treatments, excisions, vein therapy, CoolSculpting, Mohs surgery.
adrenalectomy, bariatric surgery, BPD/DS, brain stereotactic radiosurgery, hormone therapy, CT scans, diabetes treatment and diagnosis, MRIs, transplants, thyroid treatments.
walk-in appointments, annual physicals, pediatric consultation, postpartum checkup, illness.
colonoscopy, endoscopy, pH monitoring, enteroscopy, gastrostomy, manometry, banding.
regular check-ins, annual physicals, referral appointments, medication adjustments, illness.
phlebectomy, biopsy, surgery, hemorrhoids, laparoscopic surgery, lung surgery, thyroid surgery, stomach surgery, hernia repair.
molecular tests, chromosomal tests, biochemical tests, newborn screening, diagnostic testing, carrier testing, prenatal testing, pre-implantation testing.
screening, routine appointments, cervical biopsy, colporrhaphy, colposcopy, dilation and curettage, endometrial ablation, endometrial or uterine biopsy, ultrasounds, hysterectomy, hysteroscopy.
chemotherapy, cancer treatment, experimental treatments, ablation therapy, biological therapy, blood transfusions, blood and bone marrow donations, transplants.
autopsies, specimen examination, tissue examination, unnatural death investigation, on-site investigations, finding reports, testimony preparation, forensic pathology, forensic medicine.
annual physicals, illness, referral appointments, follow-up appointments.
individual counseling, couples counseling, intake surveys, assessments, interventional appointments, group counseling.
dialysis, hemodialysis, peritoneal dialysis, kidney biopsy, kidney transplant, hypertension treatment, mineral bone disorder treatment, kidney stone treatment.
brain surgery, botox injections, brain rehabilitation, carotid angioplasty, carotid stenting, concussion testing, screening, deep brain stimulation, spinal cord injury rehabilitation, spasticity treatment and management, locomotor training.
LASIK, PRK, cataract surgery, glaucoma surgery, annual examination, vision testing, screening, diabetic retinopathy, macular degeneration screening and treatment.
consultation, rehabilitation, arthroscopy, meniscectomy, decompression, carpal tunnel treatment, knee and hip replacements, ACL reconstruction, cartilage repair, physical therapy.
X-rays, CT scans, MRIs, mammograms, ultrasounds, diagnostic imaging, screening.
AI-Driven, Human Reviewed.
Better Claims. Increased Revenue. Less Burnout.
Experience the Future of Clinical Documentation
Seamless Documentation
Our HIPAA-compliant, cloud-based platform transforms dictated notes into structured medical documentation quickly and accurately. No more time-consuming EHR data entry.
Enhanced Workflow Efficiency
ZyDoc integrates effortlessly with most EHR systems, ensuring orthopedic specialists can access, review, and sign off on patient notes with minimal disruption.
AI-Powered Speech Recognition
Our advanced AI technology understands complex orthopedic terminology, significantly reducing documentation time while maintaining 99% accuracy with human experts-in-the-loop.
Reduced Administrative Burden
By leveraging ZyDoc services, orthopedic practices can enhance productivity, minimize burnout, and improve the overall patient experience.
Compliance & Security
With HIPAA-compliant encryption and secure cloud storage, your data is protected while remaining accessible anytime, anywhere.
Proven Success
Through our landmark NIH Columbia University study, ZyDoc users saved 76% on documentation costs & 61% in time savings.


Cost EHR Documentation

Documentation Time (min)

Positive Usability Measures



Choose the Smarter Path to Clinical Documentation
Unlike typing, scribes, or speech recognition, ZyDoc doesn’t just capture your notes — it inserts them directly into the correct fields of your EHR. That means faster workflows, fewer errors, and no copy-and-paste. With minimal training and setup, ZyDoc delivers high adoption, superior accuracy, and seamless usability while lowering HR demands, IT support, and physician burnout.
- Minutes to train, not weeks
- Low cost, high adoption
- Direct EHR insertion competitors can’t match
