What Is Digital Medical Transcription?
Oct 03, 2019 | Jonathan Maisel

Doctors and other health care providers have a lot to do and few moments to spare. Their days are packed with appointments that often run long and hours of data entry clicking and typing in the EHR don’t help. Or maybe an emergency comes up and requires a reshuffling of all the day’s tasks.
Digital medical transcription makes the lives of health care professionals easier. It eliminates tedious EHR data entry and allows these busy health care providers to get back to doing what they do best — caring for patients. Digital medical transcription is popular and continues to expand worldwide. The global market for medical transcription is currently valued at $5 billion and is expected to hit almost $7 billion by 2024.
What Is Medical Transcription?
Here’s a quick definition of medical transcription: It’s the process of turning health care professionals’ notes into a formal written record.
Health care providers are responsible for notes ranging from initial patient histories to summaries of the visit detailing the conversations they had with patients, along with their diagnoses, prescriptions and their recommendations for follow-up care. They also make notes about any surgeries or other clinical procedures performed. Often, they use audio recorders, telephones or even smartphone apps to dictate notes.
The notes medical professionals dictate need to be detailed. They describe the details of their office visits and examinations as well as their hospital rounds and emergency clinic visits. They summarize the findings of any blood tests, cultures, labs or radiographs. They also record vital signs and give the details of a hospital patient’s chart. If they operated or performed any outpatient procedures, such as a biopsy or endoscopy, they describe their methods and findings. These notes are needed for providing medical care, supporting billing claims, and defending against malpractice actions. Moreover, there is an increasing demand for patients to receive their medical records and the explanations and instructions have to be clear and simple so they can understand and comply with treatment recommendations to achieve positive outcomes.
An audio recorder or smartphone app is easy to use in the moment because the doctor or nurse practitioner can speak into the device while doing other things, saving time. The average doctor in the United States speaks at about 100- words per minute and can document a typical one-page short encounter in 3 minutes, leaving more time to interact with the patient to improve their experience. Many doctors also prefer to use an audio recorder or an audio app rather than write out a detailed set of notes because writing notes at 20 words a minute is significantly more time-consuming work and leaves less time to spend seeing patients.
Late, audio recording can be converted into a perfectly formatted note, letter or inserted into the appropriate sections of an EHR with accuracy approaching 99.6% due to the transcriptionist expert knowledge. Health care providers must turn their dictated notes into full written records for the practice’s use, for the use of any specialists to whom patients may be referred and for insurance companies’ use in processing claims.
Transcription work can typically take three to four times the length of a dictation and takes hours of a day. Sometimes doctor’s offices hire a separate professional transcriptionist, but these services can be expensive, especially since the doctor may not even be in the office. In-house transcription can also contribute to errors if the transcriptionist is unfamiliar with medical terminology and procedures. Specially trained medical transcriptionists exist, but they are even more expensive to hire as in-house employees and require HIPAA training, encrypted computers, desk space and management.
But because having detailed medical documentation is crucial for giving patients the care they need, someone must do the transcriptions promptly, no matter how tedious the work is and promptly varying workloads. Having accurate, thorough transcriptions is vital to making sure that providers don’t miss crucial elements in patient diagnoses or treatment recommendations. Thankfully, companies like ZyDoc offer medical transcription services that easily fit into working health care professionals’ existing workflows and can handle fluctuations in workloads, overflow, STAT jobs and are available 24/7/365 for urgent work.
Benefits of Outsourcing Medical Transcription
Outsourcing medical transcription tasks provides a multitude of benefits to health care professionals.
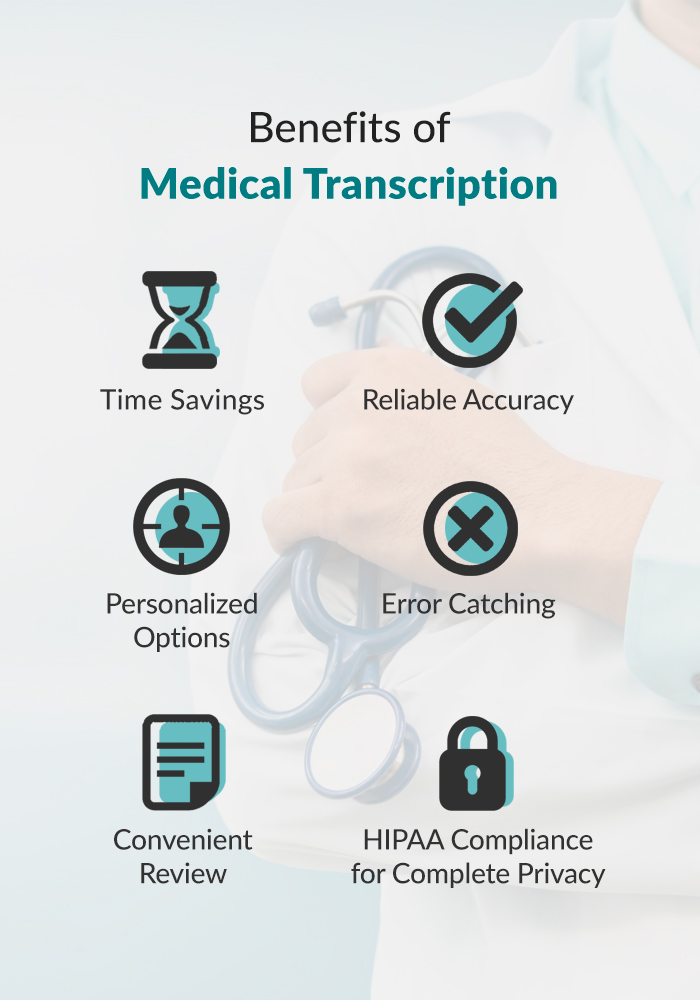
1. Time-Saving
One main advantage of digital medical transcription is the time it saves. With digital transcription, no doctor, nurse practitioner or medical assistant has to sit down with an audio file — or huge backlog of audio files — and painstakingly transcribe the notes word for word. Instead, a medical transcription service with trained professionals can use those audio files and transcribe them for health care providers with rapid turnaround times.
2. Reliable Accuracy
Digital medical transcription also offers the benefit of its accuracy. This accuracy comes in two forms. First, when you use a professional medical transcription service, you’re getting the services of highly trained professionals. These professional medical transcriptionists are well versed in medical terminology, dosages and procedures. Though health care providers can and should review the end product, their precise documentation will never be lost in the translation of a layperson.
Second — have you ever dictated a perfectly logical sentence into your phone only to have it spit out some inane speech-to-text rendering? The issue is compounded with hyper-specialized medical terminology. Digital medical transcription dramatically reduces the likelihood of garbled meaning because it does not rely on voice recognition. The trained professional transcriptionists who work on each project listen for nuance and context that voice recognition programs simply have not yet mastered. In addition, continuously using the same qualified team of transcriptionists and U.S. editors makes them familiar with each doctor and the work is returned faster and with more accurately.
Multiple studies consistently show that the error rate of voice recognition software in medical settings is 7%, with 5.7% of those errors being clinically significant. As a result, these percentages mean that of every page generated with voice recognition software, there will be an error that will likely end up negatively impacting patient outcomes. By contrast, with transcription services, the average accuracy is 99.6% (or a rate of error is 0.4%), which drops to 0.3% after physician review. With transcription services, significant errors become extremely statistically unlikely.
When patient histories, laboratory findings, surgical reports, and patient health are on the line, accuracy is vital. A simple mistake, such as hearing “enuresis” for “anuresis,” or or “galactorrhea” for “galacturia,” or “ileum” for “ilium,” could contribute to a botched treatment plan rather than an accurate diagnosis. Or if the automated voice recognition service hears “80 units of insulin” instead of “8 units of insulin,” the patient in question could be headed for a brain-damaging hypoglycemic episode rather than a speedy recovery. For this reason, it’s best to go with a transcription service you can trust for accuracy and reliability.
3. Personalized Options
Additionally, many transcription services offer different tiers of editing and quality control so that health care providers can choose the level that best fits their needs. For example, for transcribing routine office visits, family practitioners might choose a first-tier typing and editing package that offers 98% accuracy — an extremely high rate and well worth the money spent. But for tertiary care specialists, where the accuracy of records is a matter of life and death, the facility might go with a premium package that guarantees 99.6% accuracy for near-flawless results and increased peace of mind. Highly accurate documents are also expected by referring physicians and engender confidence and more referrals. Near-perfect documents are also expected by referring physicians and engender confidence and more referrals.
4. Error Catching
Trained human transcriptionists can also act as a backup set of ears in case the health care practitioner makes a mistake during dictation. A medical assistant might not have the level of knowledge necessary to catch the error. Certainly, voice recognition services could not give this feedback. But medically trained transcriptionists can alert providers to potential mistakes and ask for clarification. For instance, they can catch dictation errors such as switching right and left sides, having patients on blood thinners during pre-op or failing to include sufficient descriptions of medical issues that are necessary for proper coding.
5. Convenient Review
When transcription is complete, the benefits of convenience are hard to overstate. If a practitioner wants to review a patient’s medical history, there’s no need to listen to a lengthy audio file and dig out the relevant material. Health care providers can simply pull up the transcription file and do a quick search for what they need.
The professional formatting of the files also lends itself to quick and convenient review. Even if the audio file that went out for transcription seemed like a daunting river of speech, the file that comes back won’t be a daunting ocean of words. It will be divided into discrete, relevant, searchable parts that make reading and finding the information easy. Transcription platforms even allow for searching for terms, certain types of encounters or finding a patient within specific date ranges.
6. HIPAA Compliance for Complete Privacy
It’s important to note that high-quality, professional transcription services, such as those provided by ZyDoc, also offer the benefit of being 100% HIPAA-compliant and secure. These services adhere to several layers of strict industry regulations and protocols, including sending and receiving files on a secured network, to ensure that patient information is kept in strict confidence. The services also provide their transcriptionists with rigorous training on compliance with the act to ensure that no breaches of patient privacy occur. The ZyDoc TrackDoc™ platform also limits access to only those people with privileges and prevents a transcriptionist from downloading the actual audio or transcript to their personal computer.
How Medical Transcription Integrates with EHRs
EHRs, or electronic health records, are now ubiquitous in medical practices. Paper files are cumbersome to store and sort through, but with EHRs, patient data is available on computer systems with just a few clicks of the mouse. This system saves health professional’s valuable time in reviewing information and makes communication between different departments much easier. Everything that providers would normally store in paper files is available on the secured network, making access easy for providers while ensuring patient privacy. For these reasons, and because of penalties, almost all doctors now use EHRs in their practices.
However, EHRs come with their own set of challenges. It takes a lot of time to enter each patient’s information into the system. Additionally, some EHR systems are designed with insurance companies rather than health professionals in mind. So doctor, nurse practitioners, and clinicians may find that some parts of their work become more difficult with the adoption of an EHR system.
The data-entry burden associated with EHRs has become a primary cause of burnout among doctors around the country. Doctors who report high use of EHRs (averaging 5.9 hours daily) also report a high sense of time pressure at work, along with significant feelings of burnout, dissatisfaction and even desire to leave the profession. Inevitably, this can affect their work and productivity.
Medical transcription software integrates seamlessly with EHRs. In many cases, medical transcription programs can automatically upload transcription files to a patient’s EHR and attach them or even insert the records into the corresponding sections of the encounter. These files can also include different types of medical transcription reports, such as radiology, pathology and laboratory reports. These automatic uploads help to alleviate some of the clerical time consumption that dogs physicians’ offices, and helps eliminate errors in choosing the wrong patient, especially when smartphones are used with apps that allow the doctor to select the patient from their schedule, dictate notes and then send them.
Additionally, many doctors, in an attempt to cut down on time spent inputting information into the EHR, turn to voice recognition apps so that they can dictate and speed along the process. As we’ve discussed above, automated dictation apps are prone to “mishearing” what people say. Using them is a prime way for errors to creep into patients’ files and potentially cause harm in the course of their medical treatment. Medical transcription solves this problem by using a team of knowledgeable, efficient, professional staff. Speech recognition typically carries a high cognitive load, and, in addition to having to manually navigate to each section and remember a string of commands, the doctor is forced to correct over 7% of the errors in the speech recognized text so it takes much longer than just dictation.
Importing completed transcription files into an EHR is simple and convenient. It allows for the creation of a complete and thorough “health story”. Once the file is imported into the system, other departments that have the correct permissions can access the file, leading to a more streamlined and efficient level of patient care. Using transcription files to fill in patients’ EHRs can also improve insurance reimbursement. If EHR documentation is robust and thorough, insurance companies have little basis on which to deny coverage of services.
To streamline their dictation for EHR purposes, providers may wish to look into services like ZyDoc’sSpeechDoc, TrackDoc and TrackDoc Connect:
- SpeechDoc™: SpeechDoc is a mobile dictation app. It allows medical professionals to use their smartphones or tablets as dictation devices and then upload the audio dictation files directly to a secure digital medical transcription network. From the secure network, professional ZyDoc transcriptionists will receive the files and work on them.
- TrackDoc™: TrackDoc is a cloud-based platform where completed transcription files are stored. Providers who have obtained permission can access these files from anywhere.
- TrackDoc Connect™: TrackDoc Connect allows for interface with a provider’s EHR system. TrackDoc can automatically insert dictation files in the relevant section of a patient’s EHR. Of course, if a practice has not converted to EHRs, ZyDoc employees can upload the files to the appropriate location in your system. There also is an option to fax in documents.
It’s important to choose a medical transcription service that is compatible with your EHR system. Shop around for a service that can work with your EHR system without causing unnecessary compatibility headaches.
How Medical Transcription Benefits Physicians and Other Medical Professionals
Digital medical transcription benefits health care professionals in a variety of ways.
1. Financial Freedom
For one thing, digital medical transcription is budget-friendly. Doctors seeing four patients an hour may bill $600/hour or their opportunity cost is $10/minute. So, while using a scribe may be faster for some tasks, the scribe has to be spoon-fed information which then still has to be reviewed. This is ultimately much more time-consuming than dictation, whereas the cost of transcription by a professional typist is negligible compared with the several minutes saved on each patient encounter. Furthermore, hiring a medical assistant at a salary of $30,000 or more per year, plus benefits, is an expense that many practices, especially newer or smaller practices, cannot afford. These assistants must receive HIPAA training, take six weeks of EHR and medical terminology training and only about a fraction of them actually achieve real productivity. Additionally, mistakes made by an entry-level medical assistant may lead to further costs to the practice. In the worst-case scenario, they can lead to serious malpractice costs. Or physicians and nurse practitioners can do the work themselves, but physician data entry takes valuable hours out of their day so they see fewer patients. These are hours when they cannot be seeing patients and bringing more money into the clinic.
Investing in digital transcription services, on the other hand, doesn’t have to cost as much. Providers can choose which level of transcription fits their needs and budget. Most digital transcription services offer their transcriptions for mere cents per line of work, with a typical encounter costing only $3.00 to $6.20 depending on turnaround time, typist requirements and EHR integration needs. This dictation, transcription and EHR insertion solution is much more cost-effective than paying an in-house assistant a full salary and benefits for the labor. The digital medical transcription service can offer this lower price because it has a whole team of employees sharing in the work and participating in the benefits program.
2. Provider Convenience
Digital medical transcription is provider-friendly. Doctors and nurse practitioners have families and interests outside of work, just like the rest of us. Traditionally, if they don’t want to eat up their practice’s valuable time by doing the grunt work of EHR data capture, and they have to do it after hours. That’s hard on their personal lives. Digital transcription services solve this problem by taking the work off their hands. All they have to do is perform a quick review when their accurate, easy-to-read transcription files come back. Dictation is a natural, easy way to tell a rich “health story” and has a much lower cognitive load than typing and clicking, having to spoon-feeding data to scribes or working with complicated speech recognition technology.
Having a cloud-based system like ZyDoc’s TrackDoc™ platform means that there is no software installation required or IT support requirements. With automated enrollment, doctors can immediately start benefitting from ZyDoc Medical Transcription and EHR solutions. They can dictate with smartphones, digital recorders or telephone and no longer be tethered to the computer. Audio files and transcriptions are available from any device with Internet access, regardless of the browser or operating system in use. Work can be shared securely with others, downloaded, printed or faxed.
3. Enhanced Patient Care
Digital medical transcription is also patient-friendly. Fast, reliable, medically-trained professional transcriptionists, along with a team of editors to act as another set of eagle eyes, make sure that patient records are accurately transcribed. This rigorous attention to detail leads to complete and correct medical records, and correct medical records lead to proper and efficient care with positive outcomes. Providing the right medical care leads to satisfied patients. Patient satisfaction is also, indirectly, a bonus for medical professionals because happy patients are more likely to come back and to leave good reviews. And good reviews bring more patients through the door.
4. Speed and Accuracy
Digital medical transcription is fast. Many transcription services, including ZyDoc, offer a guaranteed rapid turnaround time on the vast majority of the projects they receive. Many transcription services also offer STAT turnaround for an additional fee.
Yet, digital medical transcription is also highly accurate. The reliable accuracy relieves doctors of the worry that they must pore over every word of an assistant’s transcription to catch errors that a trained eye should have spotted. It also relieves doctors of the worry that they will fall victim to malpractice suits because of scribe or voice-recognition transcription errors.
5. Efficiency
Using medical transcription services means improved office efficiency through better record keeping. It streamlines the record-keeping process and allows medical professionals to concentrate more of their efforts on the critical job of helping patients and saving lives. And, with up to 61% less documentation time than with keyboard and mouse, they can start seeing more patients and avoid staying late.

Start a Free Trial of Medical Transcription Services with ZyDoc
ZyDoc offers a free trial of medical transcription services, so you can try before you buy. Figure out if digital medical transcription is right for you with no payment for 14 days. Small practices with five or fewer physicians can self-enroll and start up immediately.
Our standard, professional and enterprise tiers offer 98%, 98.6% and 99% guaranteed accuracy, respectively, and our rapid turnaround times will keep your office functioning smoothly and efficiently. Our fast and efficient services are easy to implement and make health care professionals more productive, which leads to healthier and happier patients. Start your free trial with us today.
Updated on October 11, 2019
